Symptoms associated with pulmonary diseases can be very lifestyle-limiting. We can provide these patients with relief from these symptoms.
Inferior Vena Cava (IVC) Filter Placement/Removal
In an inferior vena cava filter placement procedure, interventional radiologists use image guidance to place a filter in the inferior vena cava (IVC), the large vein in the abdomen that returns blood from the lower body to the heart. The most common approach is to gain access to the jugular vein in the neck, using ultrasound guidance initially.
Blood clots that develop in the veins of the leg or pelvis, a condition called deep vein thrombosis (DVT), occasionally break up and large pieces of the clot can travel to the lungs. An IVC filter traps large clot fragments and prevents them from traveling through the vena cava vein to the heart and lungs, where they could cause severe complications or even death.
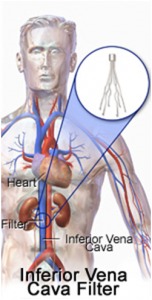
Filter Placement/Removal
Until recently, IVC filters were available only as permanently implanted devices. Newer filters, called optionally retrievable filters, may be left in place permanently or have the option to potentially be removed from the blood vessel later. This removal may be performed when the risk of clot travelling to the lung has passed. Removal of an IVC filter eliminates any long-term risks of having the filter in place. It does not address the cause of the deep vein thrombosis or coagulation. Your referring physician will determine if blood thinners are still necessary. However, not all retrievable IVC filters are able to be retrieved. These filters can be safely left in place as permanent filters.
Removal of an IVC Filter can be as easy as placing one. Using ultrasound guidance, the physician will access the jugular vein. In order to grab the filter, a snare or retrieval device is used to pull it out through the access sheath.
Read what our patients are saying!
"My sister's needs was their first priority and they was very helpful over the phone. She was seen within 15-20 minutes before I completed her paperwork. The facility was very clean and accommodating for wheelchair access. The staff was very friendly and her doctor as well. She received follow up calls and asked you to call them if my sister experience any problems."
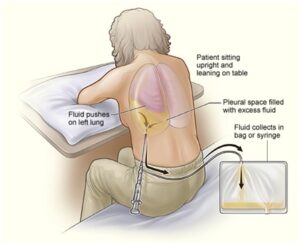
Thoracentesis
Thoracentesis is a procedure to remove excess fluid in the space between the lungs and the chest wall. This space is called the pleural space.
Normally, the pleural space is filled with a small amount of fluid—about 4 teaspoons full. Some conditions—such as heart failure, lung infections, and tumors—can cause more fluid to build up. When this happens, it’s called a pleural effusion. A lot of extra fluid can press on the lungs, making it hard to breathe.
Tunneled Pleural Catheter Placement/Removal
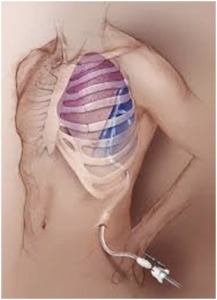
Placement/Removal
A tunneled pleural drainage catheter is a thin plastic chest tube that is placed into the pleural space by tunneling it (placing it) under the skin of your chest.
This catheter is a treatment option for removing continual accumulations of fluid within the pleural space due to conditions such as infections, metastatic cancers, liver disease or advanced congestive heart failure. It is tunneled under your skin for long-term use (weeks to months) in removing pleural fluid.
The advantage of this catheter is that it avoids the need for repeated pleural tap procedures for the removal of the re-accumulating pleural fluid. This catheter also provides a simple way for draining the pleural fluid at home on a regular, often daily, basis.
Who are Good Candidates for Pulmonary Services in Waldorf, MD?
Anyone who experiences a chronic pulmonary disease of any kind would be an ideal candidate for pulmonary services. Just a few examples of these conditions include but are not limited to ones like:
- Cystic fibrosis.
- Sarcoidosis.
- Long-form COVID.
- Emphysema.
- Bronchitis.
- Scleroderma.
Additionally, people who have had lung cancer or who have gone through various types of lung-related surgeries would also be ideal candidates for pulmonary services. This includes individuals who are about to undergo lung transplants and those who have already done so, as well as patients who have had lung volume reduction surgery.
The Benefits of Pulmonary Services
Depending on the issues that someone is facing, pulmonary services can assist in a variety of different ways. For many people, it can help them with their breathing. Ongoing pulmonary services also help increase a person's endurance and exercise tolerance.
Over the long term, this can help people tackle day-to-day activities far easier than they can currently do. Furthermore, it can also reduce the frequency of hospital visits as well.
Pulmonary services can have a significant impact on a person's mental health. Many people report feeling reduced symptoms of depression and lower levels of anxiety as well. That is why it is important to enlist the help of an experienced pulmonary team who can help you regain a higher quality of life.
The Potential Risks of Pulmonary Services
According to one recent study conducted by American Family Physicians, the risk of experiencing some type of pulmonary complication after surgery, in particular, is estimated to be between 1% and 23%.
Potential risks and complications can include the following:
- Pneumonia.
- Pulmonary edema.
- Atelectasis.
- Aspiration.
- Respiratory failure.
- Acute respiratory distress syndrome.
- Pulmonary embolism.
Myths and Misconceptions Regarding Pulmonary Services
One of the biggest myths about pulmonary services is that they are essentially the same thing as physical therapy. In reality, physical therapy is designed to help someone regain mobility or rehabilitate after an injury that they have sustained to a specific part of the body. Pulmonary services, on the other hand, are intended to help maximize someone's cardiovascular function, which can be reduced due to injury or surgical intervention.
Pulmonary Services: Recovery and Outlook
According to the Cleveland Clinic, people tend to spend between two and three days in the hospital after going through pulmonary services like a lung resection. After surgery, many patients feel a shortness of breath that will eventually subside. A big part of the recovery process will be learning coughing or deep breathing exercises. This will help patients keep their lungs clear. They may also be given supplemental oxygen to help make sure the recovery process goes as smoothly as possible.
If you'd like to find out more information about what impact the right pulmonary services can have on your life, or if you're looking for a board-certified pulmonologist near Waldorf, MD, but aren't sure where to begin, please don't delay - contact the Metropolitan Vascular Institute today or call 301-374-8540 to schedule your free consultation.

