At the Metropolitan Vascular Institute, we are equipped to manage many of your GI diseases and GI related symptoms. We can place long-term feeding tubes, help alleviate pain and discomfort from liver or gallbladder obstruction, and manage the removal of ascites (fluid in the belly).
Paracentesis
Paracentesis is a procedure in which fluid from the abdomen is removed through a needle. There are two reasons to take fluid out of the abdomen; one is to analyze it, the other is to relieve pressure. The liquid that accumulates in the abdomen is called ascites. Ascites seeps out of organs for several reasons related either to disease in the organ or changing fluid pressures. This procedure is performed using local anesthesia and ultrasound guidance. In some cases this procedure may be repeated, sometimes even weekly, to provide the patient with relief from their discomfort.
Tunneled Peritoneal Catheter Placement/Removal
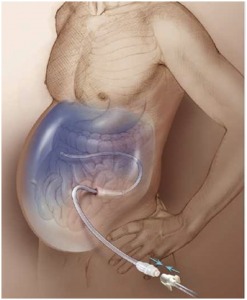
Placement/Removal
Tunneled peritoneal catheter insertion is performed as a treatment option for recurrent ascites (fluid in the abdomen). Patients with metastatic cancers or liver disease are typically candidates for this procedure. Patients with ascites due to cancer are able to have a tunneled peritoneal catheter placed to relieve their abdomen fullness, pain, and breathing issues. This procedure is performed using conscious sedation, ultrasound and x-ray guidance. The patient can connect the tunneled catheter to disposable drainage bottles, at home. This eliminates repeated office visits to have their fluid drained.
Percutaneous Gastrostomy Tube Placement/Changes
A gastrostomy is a direct opening from your abdominal wall into your stomach through which you can be fed. This procedure is performed when you cannot swallow, either because you have had a stroke, or you have developed another problem that makes it hard for you to swallow. Most of the time gastrostomy is a temporary measure, but sometimes it is permanent.
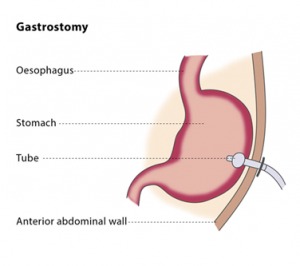
Placement/Changes
The procedure is performed using conscious sedation. Air is placed into the stomach so that it can be easily accessed percutaneously (through the skin) and better visualized under fluoroscopy. In order to achieve this, we will place a small catheter through the nose and into the stomach by passing it down the esophagus. Once the stomach is “inflated”, access is gained with a needle and a guide wire. This access is converted into a feeding tube. Exchanging a gastrostomy tube is easily done using a guide wire. A tube may need to be exchanged if it becomes clogged or if it breaks.
Cholecystostomy Tube Placement/Changes
A cholecystostomy is a procedure where a stoma is created in the gallbladder, which can facilitate placement of a tube for drainage. It is sometimes used in cases of cholecystitis, where the patient is critically ill, or if there is a need to delay cholecystectomy (surgical removal of the gallbladder). After the patient’s symptoms resolve and his/her condition is stabilized, definitive treatment is still gallbladder removal.
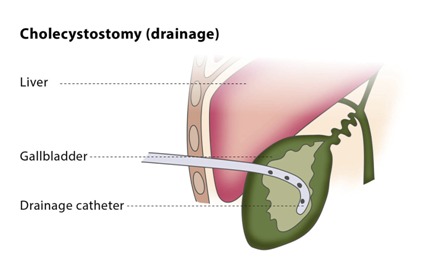
This procedure is performed using conscious sedation. The drainage catheter is placed once access to the gallbladder is achieved with a needle and guide wire. Access is easily accomplished using ultrasound and x-ray guidance.
Exchanges of these drainage catheters may be necessary if they become clogged and stop draining. This is a quick, straightforward procedure, and can be done using a guide wire.
Why Choose Metropolitan Vascular Institute?
The Metropolitan Vascular Institute was created as a multi-discipline practice with a wide range of expertise through our various providers. Our seven board-certified doctors and surgeons are certified in general surgery, vascular surgery, vascular and interventional radiology, and diagnostic and interventional nephrology. Our four nurse practitioners also have individual areas of specialization.
We provide this spectrum of medical expertise and treatment in our newly built, state-of-the-art outpatient center in Waldorf. This facility provides our patients with a relaxed outpatient environment where we where we can provide a comprehensive scope of care.
How Do I Get Diagnosed for My Gastrointestinal Problem?
At Metropolitan Vascular Institute, we pride ourselves on being available for our patients. You can expect to be able to schedule same day or next day appointments in most cases.
Our diagnosis will start with your symptoms, description when your pain began, and your medical history. For instance, pressure in the abdomen could be a sign of paracentesis.
How Will My Peritoneal Dialysis Catheter Be Removed?
A peritoneal dialysis (PD) catheter is a special tube that is inserted into the patient’s abdominal cavity for delivery of the dialysate during peritoneal dialysis. The dialysate absorbs waste products from blood vessels in the patient’s abdominal lining (peritoneum) and then is drawn back out of your body and is discarded.
Patients need to have their PD catheter removed for these reasons:
- Following a successful kidney transplant
- Changing the type of dialysis to hemodialysis
- If the PD catheter fails to work
- In the event of an episode of peritonitis that does not respond to antibiotic treatment
- If you develop a tunnel or exit site infection that does not respond to antibiotic treatment
The PD catheter can be removed in two methods. The “pull” method is the simplest and creates minimal recovery. These are performed with the patient under local anesthetic (although you are prepped for general anesthesia in case this method is unsuccessful in removing the catheter). The procedure doesn’t require any incisions to be made. The catheter is simply “pulled” out, leaving the catheter cuffs in your tissue under the skin, which will form scar tissue later. These are simple procedures that take just a few minutes.
In some patients, the “pull” method is not appropriate, so minor surgery is necessary. The patient is placed under general anesthesia and your Metropolitan Vascular Institute vascular surgeon will make a couple of small incisions to access and remove the catheter. During the procedure a small cut is made (about 2-3 inches) near the belly button. Your surgeon will carefully detach the catheter cuffs, which hold the catheter in place from the surrounding tissue. Once the catheter is removed the incision is closed with stitches, staples, or surgical glue. This method is also used if the “pull” method is unsuccessful.
How Do I Care for My Percutaneous Endoscopic Gastrostomy Tube?
A percutaneous endoscopic gastrostomy (PEG) is a procedure to place a feeding tube. These feeding tubes are typically known as PEG tubes, and they allow the patient to receive nutrition directly through their stomach. This is necessary when patients have difficulty swallowing for reasons such as a brain injury, stroke, or cancer.
Keeping a PEG tube clean and in good working order is important. Here are tips for this care:
- Always wash your hands before and after each use to help prevent infections.
- Always flush your PEG tube before and after each use. This helps prevent blockage from formula or medicine. Use at least 30 milliliters of water to flush the tube.
- If your PEG tube becomes clogged, try to unclog it as soon as you can. Flush your PEG tube with a 60 ml syringe filled with warm water. Don’t use a wire to unclog the tube, as this can poke a hole in the tube.
- Check the PEG tube daily:
- Check the length of the tube from the end to where it goes into your body. If this length increases, this could indicate the tube is coming out. If it shortens, you need to call us at Metropolitan Vascular right away.
- Check the bumper. The bumper is a piece that goes around the tube, next to your skin. It should be snug against your skin. If it is too tight or too loose, we need to know right away.
- Use an alcohol pad to clean the end of your PEG tube. Clean before you connect tubing or a syringe to your PEG tube and after you remove it. Do not let the end of the PEG tube touch anything.
How Do I Care for The Skin Around My Peg Tube?
- Clean the skin around your tube 1 to 2 times each day. Check for redness, swelling, or pus in the area where the tube enters your body. Check for fluid draining from your stoma (the hole where the tube was inserted).
- Gently turn your tube daily. This may decrease pressure on your skin under the bumper. It also helps to prevent infection.
- Keep the skin around your PEG tube dry. This helps prevent infection and skin irritation.
Are There Possible Complications from Peg Tubes?
Possible risks of percutaneous endoscopic gastrostomy include:
- Accidental tube dislodgement (tube moving out of place or coming out)
- Aspiration (accidentally inhaling your stomach contents)
- Infection near the incision
- Pain near the PEG tube
- Stomach leakage around the tube
Patient Testimonial
"My sister's needs was their first priority and they was very helpful over the phone. She was seen within 15-20 minutes before I completed her paperwork. The facility was very clean and accommodating for wheelchair access. The staff was very friendly and her doctor as well. She received follow up calls and asked you to call them if my sister experience any problems."
Schedule a Waldorf Gastrointestinal Consultation Today
To schedule a consultation or make an appointment in Waldorf, please call us at (301) 374-8540 or fill out an online contact form and our office will in touch with you. Thank you for choosing Metropolitan Vascular Institute in Waldorf, MD!

