Hemorrhoids (HEM-uh-roids) are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids may result from straining during bowel movements or from the increased pressure on these veins during pregnancy.
What are hemorrhoids?
Hemorrhoids (HEM-uh-roids) are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids may result from straining during bowel movements or from the increased pressure on these veins during pregnancy.
Hemorrhoids may be located inside the rectum (internal hemorrhoids), or they may develop under the skin around the anus (external hemorrhoids). The cause of hemorrhoids may also be idiopathic or unknown
What are the Common Symptoms of Hemorrhoids?
- Painless bleeding during bowel movements — you might notice small amounts of bright red blood on your toilet tissue or in the toilet
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- A lump near your anus, which may be sensitive or painful (maybe a thrombosed hemorrhoid)
- Hemorrhoid symptoms usually depend on the location.
What are the Different Types of Hemorrhoids?
There are two main types of hemorrhoids, internal and external. Within these two main categories, there are prolapsed hemorrhoids and thrombosed hemorrhoids.
Internal hemorrhoids may develop farther into the anal canal, where they protrude from the wall of the canal or the rectum. Internal hemorrhoids may prolapse, meaning that they swell and lengthen to a point at which they protrude to the outside of the anus. Prolapsed hemorrhoids may protrude only under strain and retract upon relaxation. In more serious cases, the protrusion may be persistent.
External hemorrhoids are visible as bumps around the anus. A thrombosed hemorrhoid is an external hemorrhoid in which blood has accumulated, causing discomfort.
What are the Causes of Hemorrhoids?
The short answer is that hemorrhoids are caused by strain on the rectum or anus. This strain causes small veins in the area to dilate and swell. Factors that can lead to strain on the small veins in these areas include:
- Straining during bowel movements
- Lack of sufficient fiber in your diet
- Chronic constipation
- Frequent diarrhea
- Not having regular bowel movements
- Pregnancy and childbirth
- Sitting for long periods
- Excess weight
- Overuse of laxatives
How are Hemorrhoids Diagnosed?
A doctor may perform a visual examination after reviewing your medical history and discussing your symptoms. Internal hemorrhoids may be diagnosed via a digital examination, in which the doctor feels the inside of the rectum using a gloved, lubricated finger. In some cases, it is necessary to use a small, flexible tube with a camera on the end to achieve a visual examination of the rectum or anal canal. Depending on your medical history and symptoms, your doctor may advise you to have a colonoscopy, a simple screening that examines the entire colon.
Are Hemorrhoids Serious?
In most cases, hemorrhoids are not considered serious. Generally, these dilated veins are so small that they don't cause symptoms. This means you can have hemorrhoids and not even know it. According to statistics, less than five percent of people who develop hemorrhoids require treatment.
What Happens if They are Left Untreated?
You may not require treatment for your hemorrhoids. They may clear up on their own after a few days. Your doctor may recommend treatment if you have prolapsed hemorrhoids that do not retract when not under strain. In this instance, the prolapsed hemorrhoids can cause significantly uncomfortable pain, bleeding, itching, and general irritation.
Are Hemorrhoids Cancerous?
No. Hemorrhoids are not cancerous and do not lead to cancer. That said, they do present similar symptoms, including pain, itching, and bleeding from the rectum. Your doctor will perform a thorough medical history and the exams and tests that can provide accurate data to reach a proper diagnosis.
How to Prevent Hemorrhoids:
Keeping your stools soft a good way to prevent hemorrhoids, so they pass easily. Additional tips:
High-fiber foods: Eat more fruits, vegetables, and whole grains. This softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
Fluids: Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
Consider fiber supplements. 25 grams a day of Fiber is recommended for women and 38 grams a day for men. Studies have shown that over-the-counter fiber supplements, such as Metamucil and Citrucel, improve overall symptoms and bleeding from hemorrhoids.
If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause constipation or make constipation worse.
Strain: Straining when trying to pass a stool creates greater stress in the veins in the lower rectum.
Urgency: Take time to have a bowel movement when you have the urge. Your stool could become dry and be harder to pass if you wait.
Exercise: Stay active to help prevent constipation and to reduce pressure on veins!
Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
Treatment Options for Hemorrhoids:
- Medications
- External hemorrhoid thrombectomy
- Rubber band ligation of hemorrhoid
- one or two tiny rubber bands around the base of internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week. This procedure is effective for many people.
- Hemorrhoid banding can be uncomfortable and may cause bleeding, which might begin two to four days after the procedure but is rarely severe. Occasionally, more-serious complications can occur.
- Injection (sclerotherapy). In this procedure, your doctor injects a chemical solution into the hemorrhoid tissue to shrink it.
- Coagulation (infrared, laser or bipolar). Coagulation techniques use laser or infrared light or heat.
- Hemorrhoid removal. In this procedure, called hemorrhoidectomy, your surgeon removes excessive tissue that causes bleeding.
- Stapling. This procedure, called stapled hemorrhoidectomy or stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids.
What is the Emborrhoid Procedure?
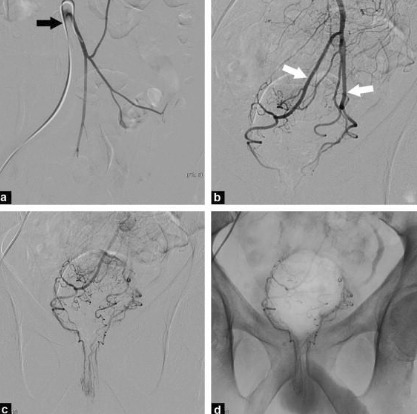
- A procedure in which a microcatheter is placed from the femoral artery (top of the leg) to the arteries of the rectum
- Small coils are inserted into the rectal arteries to decrease the flow to the hemorrhoids, also allowing for a reduction in pressure to the area.
Angiographic evaluation of the superior rectal arteries is performed from the wrist or from a femoral approach. After identifying abnormally dilated vasculature, the distal superior rectal arteries are treated with coil embolization.
About Your Emborrhoid Procedure:
- Outpatient procedure
- Performed under ‘twilight sleep’ without the need for anesthesia
- Painless procedure, with NO incisions
- Approximately 1 hour
- No need for foley catheter
- Rare complication rate
- No reports of incontinence after
- Symptom improvement occurs 2-3 weeks after the procedure
Schedule Your Consultation Today!
Call (301) 374-8540 to schedule your consultation with our providers today! Metropolitan Vascular Institute serves Waldorf, MD & all nearby areas.

