Peripheral Vascular Disease (PVD) is a circulation disorder that affect blood vessels outside the heart and brain. PVD that develops only in the arteries is called Peripheral Arterial Disease (PAD). PAD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries.
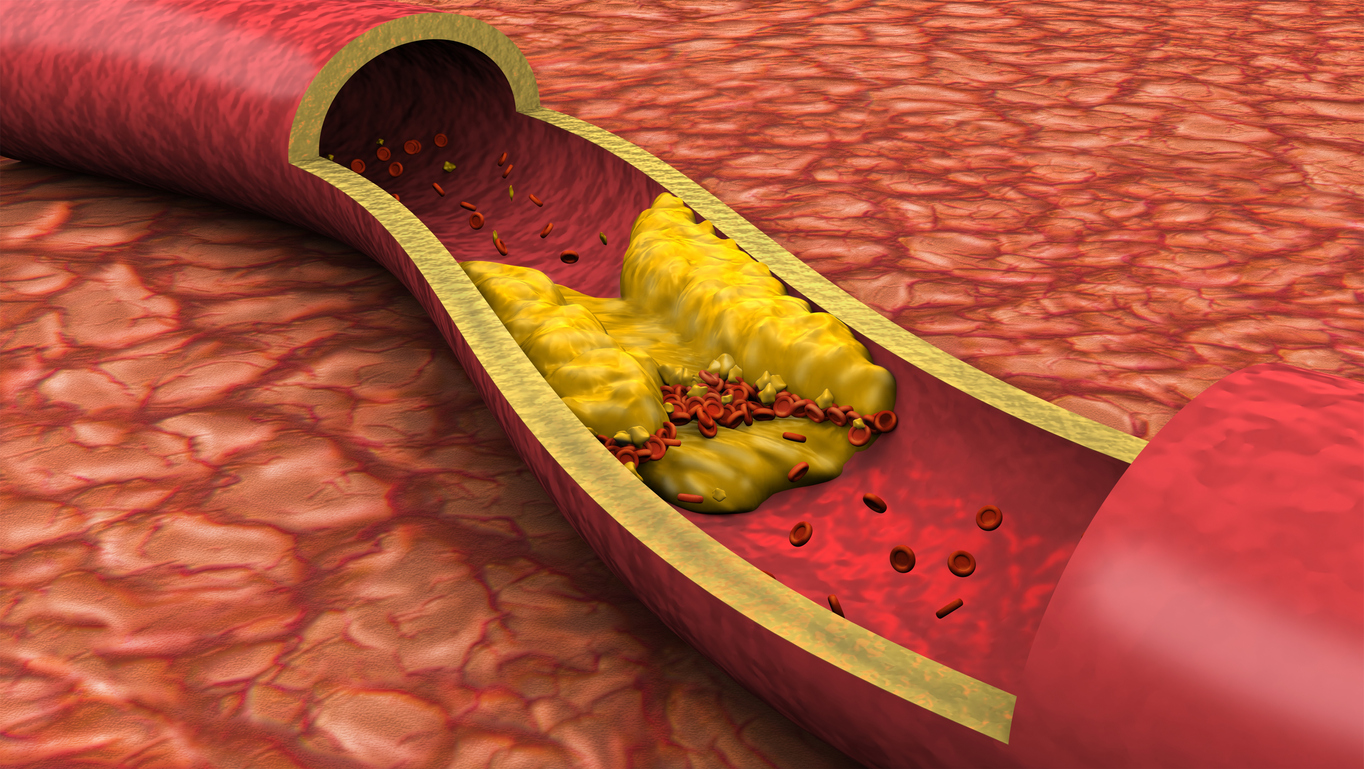
This is a very serious condition. The clogged arteries cause decreased blood flow to the arms, or more commonly, the legs. This can result in pain when walking and eventually gangrene and/or amputation.
*Rights reserved with the owner of the video
Signs and Symptoms:
The most common symptom of PAD is called intermittent claudication, which is painful cramping in the leg or hip that occurs when walking or exercising and typically disappears when the person stops the activity. Other symptoms include: numbness, tingling and weakness in the lower legs and feet, burning or aching pain in feet or toes when resting, sore on leg or foot that won’t heal, cold legs or feet, color changes in skin of legs or feet, hair loss on legs, pain in the legs or feet that wakes you up at night.
PVD that develops in the deep veins in the body is usually caused from claudication and is called Deep Vein Thrombosis (DVT).
Diagnosis:
In order to diagnose PVD, the physician will begin by taking a complete medical history and physical exam. Several tests may be used to diagnose PVD. They are:
- Measuring the pulses in your legs and feet
- Doppler ultrasound
- Ankle-Brachial Index (ABI)
- Pulse Volume Recording (PVR)
- Angiography
Patient Testimonial
"Friendly, courteous, professional. This is the absolute best medical staff in the Fredericksburg area for this medical specialty. Anyone with a vascular condition please do yourself a favor and call them."
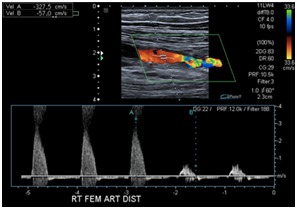
Arterial Duplex Ultrasound Scan
An Arterial Duplex Ultrasound is a non-invasive imaging scan that uses sound waves to create a color map of the arteries in your leg(s) to identify narrowing of your vessels that may be causing leg pain when walking or at rest, ulcers of the foot, ankle, heel or toe(s), or skin discoloration.
Peripheral Angiograms:
Abdominal aortograms with runoff are arteriograms of the lower abdominal aorta and arteries in the legs. This exam is often done when the patient has pain in the calf muscle after walking a short distance, discoloration of the toes or feet, non-healing wounds or ulcers, or a “cold” foot.
Treatment Options:
Once angiographic images have been obtained and problem areas identified, some of the methods we utilize to treat those diseased areas are Angioplasty, Thrombectomy, Atherectomy, or Stent placement.
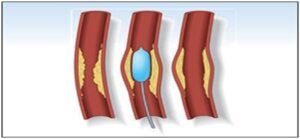
Angioplasty uses a balloon catheter to open up a stenotic area (or area of narrowing) in a blood vessel.
Thrombectomy is a process in which thrombus (or clot) is mechanically removed from the body using specialized equipment.
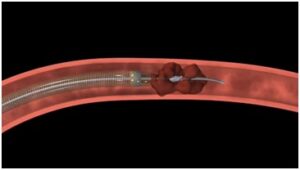
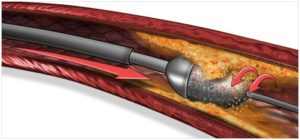
Athrectomy refers to the mechanical removal of atheroma or atherosclerosis from the inside of the vessels in the body, using specialized catheters and equipment.
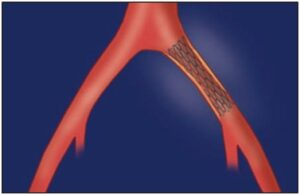
Stents are small metal scaffolds that can be placed in order to maximize the inner diameter of vessels and help to keep it open.
What Are the Symptoms of Peripheral Arterial Disease?
One of the most common symptoms of PAD is intermittent claudication, or painful cramping in the legs or hip that occurs during walking or exercising and disappears as soon as the activity is stopped. Other symptoms of PAD include numbness, tingling, and weakness in the lower legs and feet, burning or aching pain in feet or toes when resting, soreness on the leg or foot that won’t heal, cold legs or feet, color changes in the skin of legs or feet, hair loss on legs, pain in the legs or feet that wakes you up at night.
What Causes PVD and PAD?
The main cause of PVD is the build-up of fatty deposits which cause the narrowing of a blood vessel or artery. Risk factors that can cause this build-up are:
- Smoking
- Regularly breathing in second-hand smoke
- Stress
- Eating foods high in saturated fats
- Lack of exercise
- Unbalanced lifestyle
How Is PVD Diagnosed?
In order to diagnose PVD, the physician will begin by taking a complete medical history and physical exam of the prospective patient. Several tests may be used to diagnose PVD such as:
- Measuring the pulses in your legs and feet
- Doppler ultrasound
- Ankle-Brachial Index (ABI)
- Pulse Volume Recording (PVR)
- Angiography
At Metropolitan Vascular Institute, we also use the following two methods to test and diagnose patients with PVD/PAD:
Arterial Duplex Ultrasound Scan
An Arterial Duplex Ultrasound is a non-invasive imaging scan that uses sound waves to create a color map of the arteries in your leg(s) to identify narrowing of your vessels that may be causing leg pain when walking or at rest, ulcers of the foot, ankle, heel or toe(s), or skin discoloration.
Peripheral Angiograms
Abdominal aortograms with runoff are arteriograms of the lower abdominal aorta and arteries in the legs. This exam is often done when the patient has pain in the calf muscle after walking a short distance, discoloration of the toes or feet, non-healing wounds or ulcers, or a “cold” foot.
How Is PVD or PAD Treated?
Once angiographic images have been obtained and problem areas identified, some of the methods we utilize to treat those diseased areas are:
Angioplasty
Angioplasty uses a balloon catheter to open up a stenotic area (or area of narrowing) in a blood vessel.
Thrombectomy
Thrombectomy is a process in which a thrombus (or clot) is mechanically removed from the body using specialized equipment.
Atherectomy
Athrectomy refers to the mechanical removal of atheroma or atherosclerosis from the inside of the vessels in the body, using specialized catheters and equipment.
Stents
Stents are small metal scaffolds that can be placed in order to maximize the inner diameter of vessels and help to keep them open.
Schedule a Client Consultation
If you are interested in learning more about Peripheral Arterial Disease (PAD) / Peripheral Vascular Diseases (PVD) and treatments, please call (301) 374-8540 to schedule a consultation!

