At the Metropolitan Vascular Institute, we are well versed in the treatment and management of urological diseases, from alleviating blockages to providing drainage.
Prostate Artery Embolization
Prostate Artery Embolization (PAE) is a minimally invasive procedure for the treatment of benign prostatic hyperplasia (BPH) with lower urinary tract symptoms (LUTS). Men suffering from urinary frequency, the frequency at night (nocturia), urinary retention, blood in the urine (hematuria), weak stream, difficulty going, and/or starting and stopping urination could potentially benefit from this procedure.
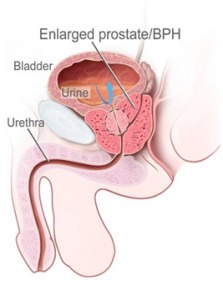
Enlarged prostate or benign prostatic hyperplasia (BPH) is the most common benign neoplasm, or new abnormal growth of tissue in men, with more than 50 percent of men aged 60–69 years and as many as 90 percents aged 70–89 years experiencing symptoms. As life expectancy increases so do the occurrence of BPH.
As a man ages, the prostate gland slowly enlarges and may press on the urethra and cause the flow of urine to be slower and less forceful.
Enlarged prostates cause urinary frequency, urgency, passing urine more often, particularly at night (also called nocturia), weakened stream and incomplete bladder emptying. Such symptoms can have significant negative impact on the quality of life, leading many men to seek treatment.
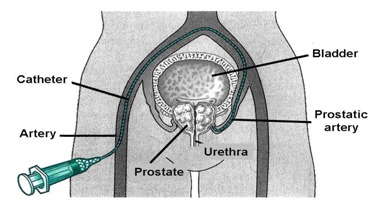
The standard treatment for BPH is surgery, which requires general anesthesia and can cause complications, such as urinary incontinence, sexual dysfunction, impotence and retrograde ejaculation, in which semen enters into the bladder. PAE, which can be performed under light anesthesia, involves a treatment called embolization, which entails temporarily blocking blood flow to the arteries that supply the prostate.
During PAE, an interventional radiologist makes a tiny incision in the groin and advances a small tube called a catheter, to the prostate artery. Microscopic beads are released into the artery, where they lodge and temporarily block blood flow to the prostate, causing it to shrink.
Frequently Asked Questions regarding PAE
How do I know if I am a candidate for PAE?
Our coordinator will send you some forms that you can fill out on the computer and send back via email. The doctor will review the information you provide and, if appropriate, a phone consultation (or in-person, office consultation) will be arranged with you.
Is the procedure covered by my insurance?
Some private insurance companies are covering the procedure. We have an in-office insurance coordinator who will take care of any necessary pre-authorizations or pre-determination letters.
Do I receive anesthesia for the procedure? Is it a painful procedure?
You will receive conscious sedation, IV medications, during the procedure to help keep you relaxed and comfortable. The procedure is not a painful one. We access the vessels that feed the prostate by way of the femoral artery in the groin.
How long is the procedure?
Procedure times do vary from patient to patient, however, on average, most last between 90-120 minutes. You will stay in our recovery area for two hours after the procedure.
Do I need to have a Foley catheter for the procedure?
No
Can I drive home?
No. You may not drive for 24 hours after the procedure. Someone else can drive you or you may travel by public transportation. If you are coming from out-of-town, we ask that you stay locally the night of the procedure. We consider this safe practice.
Do I need to get blood work or any other pre-procedure tests/exams before my PAE?
This will be determined at the time of your initial consult with the doctor. It is possible that he may ask for blood work or a special CT scan prior to moving forward with the PAE.
Are the embolization particles permanent?
Yes, the particles are permanent.
Do the particles move? Ever go somewhere unintended?
With our doctor’s expertise and extreme attention to detail, the particles are only delivered to their intended target arteries. Once delivered, the particles do not move.
Are there additional charges for follow-ups?
No. All follow-ups are included.
When can I return to work/physical activity/sexual intercourse?
Avoid strenuous activity, such as climbing long flights of stairs, for 24 hours after your procedure. No heavy lifting (greater than 10-20 lbs) for a week, or until the puncture site heels. Upon resuming sexual intercourse, be aware that you may see blood in your ejaculate for 7-21 days.
See What Our Patients Are Saying...
"My experience with MVI has been a wonderful experience I have the pleasure of being the patient of Dr. Wu and Dr Gupta and their staff. They have been nothing short of a miracle. Their attentiveness and care for the patient is felt when you first meet them and I love it and the choice I made. Thank you and keep up the great work."
Varicocele Embolization
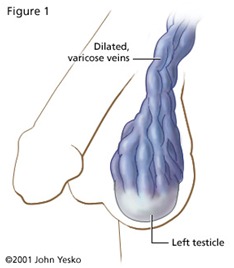
A varicocele is a varicose vein of the testicle and scrotum that may cause pain, infertility in men, and possibly lead to testicular atrophy (shrinkage of the testicles). It is a condition that affects approximately 10 percent of men. In healthy veins within the scrotum, one-way valves allow blood to flow from the testicles and scrotum back to the heart. In a varicocele, these valves do not function properly and sometimes fail. This can cause a reverse flow of blood which stretches and enlarges the tiny veins around the testicle. This tangled network of blood vessels, or varicose veins, is called a varicocele.
What are varicocele symptoms?
Typical symptoms are mild and many do not require treatment. Treatment may be necessary if the varicocele is causing discomfort or any of the other problems listed below.
- Pain: One of the signs of varicoceles is an aching pain when the individual has been standing or sitting for an extended time and pressure builds up in the affected veins. Heavy lifting may make varicocele symptoms worse and, in some cases, can even cause varicoceles to form.
- Fertility Problems: There is an association between varicoceles and infertility or subfertility, but it is difficult to be certain if a varicocele is the cause of fertility problems in any one case. In one study, as many as 40 percents of men who were subfertile were found to have a varicocele. Other signs of varicoceles can be a decreased sperm count; decreased motility, or movement, of sperm; and an increase in the number of deformed sperm. It is not known for sure how varicoceles contribute to these problems, but a common theory is that the condition raises the temperature of the testicles and affects sperm production. Studies have shown that 50-70 percent of men with fertility problems will have a significant improvement in the quality and/or quantity of sperm production after they have undergone varicocele repair.
- Testicular Atrophy Atrophy, or shrinking, of the testicles is another sign of varicoceles. The condition is often diagnosed in adolescent boys during a sports physical exam. When the affected testicle is smaller than the other, treatment is often recommended. The repaired testicle will return to normal size in many cases.
How are varicoceles diagnosed?
Sometimes a varicocele can be diagnosed during a physical examination. A large varicocele may make the scrotum look lumpy so it resembles “a bag of worms” (see Figure 2).
When varicocele symptoms are not clearly present, the abnormal flow of blood can often be detected with a noninvasive imaging exam called color flow ultrasound. Varicoceles also may be detected with a venogram – an x-ray in which a special dye is injected into the veins to “highlight” blood vessel abnormalities.
What are my treatment options?
In the United States, varicocele treatment has traditionally involved open surgery, usually performed by a urologic surgeon, or urologist. In recent years, however, a safe and effective nonsurgical alternative called varicocele embolization is becoming the treatment of choice for many patients and their physicians.
Varicocele Embolization:
Varicocele embolization is a minimally invasive procedure performed by an interventional radiologist, and is as effective as surgery with less risk, less pain and less recovery time. Patients considering surgical treatment should also get a second opinion from an interventional radiologist to ensure they know all of their treatment options.
Unlike varicocele surgery, embolization requires no incision, stitches, or general anesthesia. In addition, embolization patients almost never require overnight admission to the hospital and several studies have shown that embolization is just as effective as surgery. Studies have also shown that embolization patients return to full activities in a day or two, but varicocele surgery patients may need to avoid strenuous activity for several days or even weeks. Some complications of varicocele surgery, such as hydrocele (fluid around that testicle) and infection are virtually unheard of after embolization.
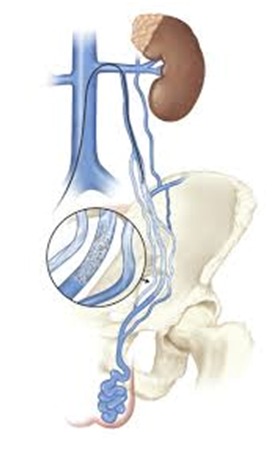
Figure- A platinum coil, delivered through the catheter, is placed in the affected vein, then a sclerosing agent is injected to block collateral veins. This helps to prevent recurrences.
During the embolization, the doctor inserts a catheter into the jugular vein, in the neck, down into the faulty vein(s). Catheterization requires only a small nick in the skin for insertion and x-ray image guidance of the catheter to its target area. The catheter delivers Dacron filaments-bearing coils that clot the blood and seal the faulty vein. The use of the recently developed Sotradecol foam agent allows the radiologist to block even the smallest veins not previously accessible.
Frequently Asked Questions regarding Varicocele:
A Varicocele is a network of tangled blood vessels (varicose veins) in the scrotum. It is a leading cause of male infertility and may also cause pain and atrophy (shrinkage) of the testicles.
Unlike varicocele surgery, embolization requires no incision, stitches, or general anesthesia. Further, embolization patients almost never require overnight admission to the hospital. In addition, several studies have shown that embolization is just as effective as surgery. Studies have also shown that embolization patients return to full activities in a day or two, but varicocele surgery patients may need to avoid strenuous activity for several days or even weeks. Some complications of varicocele surgery, such as hydrocele (fluid around that testicle) and infection are virtually unheard of after embolization.
Not necessarily. If you have symptoms, such as pain, you may choose to have a varicocele repair procedure sooner. But an asymptomatic varicocele is a common condition that does not necessarily cause pain or infertility. A varicocele only needs to be fixed when it causes pain, shrinkage of a testicle, or when it is associated with male infertility.
Many studies have shown that varicocele repair can improve semen analysis significantly, but there is no guarantee that any individual patient will experience a significant improvement. Pregnancy rates in infertile couples improve after varicocele repair by about 30-50%.
Successful varicocele repair reduces the swelling and discomfort of symptomatic varicoceles. There are other causes of scrotal pain that may need to be ruled out before varicocele treatment.
Minor complications such as bruising at the catheter site, nausea or low-grade backache may occur, but are uncommon. Infection, hydrocele or loss of a testicle has not been reported after coil embolization.
The procedure is performed with local anesthesia and “twilight” sedation. It is not a painful procedure. In one study, patients who underwent both varicocele surgery and embolization for varicocele repair, overwhelmingly favored embolization.
Typically, patients are observed for a few hours and go home the same day.
Patients are instructed to rest quietly at home on the day of the procedure. They may resume normal activity the next day. Varicocele surgery often has a longer recovery time.
While every patient is different, recovery from varicocele embolization typically takes less than 24 hours and many patients return to work the next day.
No.
There is a 5-11% chance that a varicocele could recur after embolization. If so, surgery may be needed. Keep in mind that a varicocele may also recur after surgery.
Yes. Embolization is a highly effective way to treat varicocele after failed surgery.
The cost is generally comparable to varicocele surgery. However, the cost varies depending on geographic area and local insurance company policies. You should contact a local interventional radiologist to discuss the cost in detail.
Generally, insurance companies will pay for the varicocele embolization if they pay for varicocele surgery. Understand, however, that some insurance companies limit the coverage provided for infertility treatment. Check with you insurance company about this policy.
Although the radiologist guides the catheter with an x-ray machine during embolization, the amount of radiation exposure to the testicle is very low – about equal to the amount received during a chest x-ray.
During varicocele embolization, no incision is made in or near the testicles. Rather, a tiny nick is made in the neck to insert a catheter (a small tube). Next, the catheter is guided down to the abdomen and into the varicocele vein. After the procedure, the catheter is removed and no stitches are needed.
Nephrostomy Catheter Placement/Exchange
Percutaneous nephrostomy (PCN) tube is a catheter (plastic tube) that is inserted through your skin into your kidney. The nephrostomy tube is placed to drain urine from your body into a collecting bag outside your body.
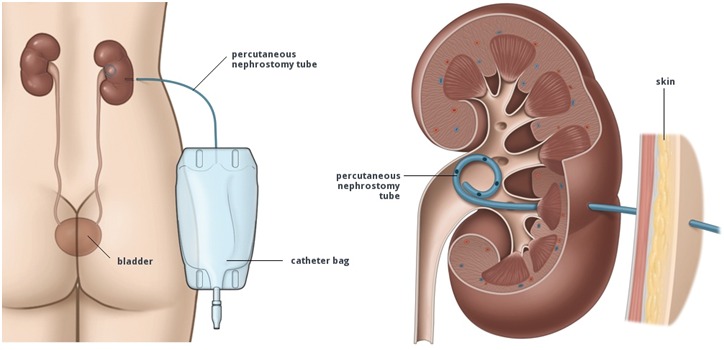
You may need a percutaneous nephrostomy tube when something is blocking the normal path that your urine takes to leave your body. Urine from your kidneys passes through thin, narrow tubes called ureters. Your ureters are connected to your bladder where urine is stored for a time before you urinate. When stones or blood clots block your ureters, urine stays in your kidneys and will cause problems. The nephrostomy tube is put into drain your urine directly from your kidneys. You may need this tube if you have pelvic tumors, damage to the urinary system, prostate cancer, or other conditions.
If you already have a nephrostomy tube in place, it should be changed routinely every three months or so. We can do that simply by cutting the suture that holds it to the skin, inserting a guide wire into the catheter, and exchanging the old catheter for a new one over the guide wire. Once the new catheter is in the correct position the guide wire is removed, the new catheter is sutured in place and connected to a drainage bag.
Suprapubic Catheter Placement
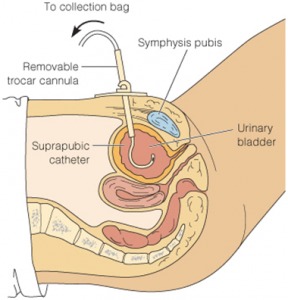
Symptomatic bladder outlet obstruction and neurogenic bladder dysfunction are common conditions, frequently requiring long-term use of indwelling bladder catheters for adequate bladder emptying, prevention of complications of long-term bladder outlet obstruction, patient comfort, and optimal quality of life.
A suprapubic catheter is placed through the skin, just above the level of the pubic bone, into the bladder to allow for drainage. In many cases, placing these catheters percutaneously allow for increased patient comfort and fewer infections when compared to traditional Foley catheters placed into the urethra.
Book a Consult at the Metropolitan Vascular Institute!
To learn more about the various Urological Services offered at our practice, or to schedule an appointment with one of our experienced and knowledgeable providers, please call (301) 374-8540 or click here to send us an appointment request form. Our practice serves Waldorf and the surrounding areas of Maryland.

